| MEDICAL INTRO |
| BOOKS ON OLD MEDICAL TREATMENTS AND REMEDIES |
THE PRACTICAL |
ALCOHOL AND THE HUMAN BODY In fact alcohol was known to be a poison, and considered quite dangerous. Something modern medicine now agrees with. This was known circa 1907. A very impressive scientific book on the subject. |
DISEASES OF THE SKIN is a massive book on skin diseases from 1914. Don't be feint hearted though, it's loaded with photos that I found disturbing. |
ANATOMY AND PHYSIOLOGY OF THE SKIN
ANATOMY
The integument is not to be viewed merely as the protective en
velope or covering of the body, but as an integral and closely associated
part of the general economy, with correlated and independent func
tions, and with duties to perform that give it a good claim to be looked
upon additionally as an independent, and probably much underrated,
organ. A proper understanding of its histologic construction and of its
important physiologic functions is necessary in order to obtain a clear
idea of the various pathologic processes that take place in its component
tissues, and the clinical external objective lesions to which they give rise.
The integument is a somewhat complex elastic fibrous structure,
enveloping the whole body, and merges into the mucous membrane,
with which it is continuous, at all the natural mucous orifices. Through
its own connective tissue, its numerous blood-vessels, nerves, lymphatics,
etc, it forms a close and firm association with the structures of the
body beneath. Although the surface is, as a whole, approximately
smooth, close inspection shows innumerable ridges, furrows, and pores,
and the presence of variously sized hairs, and, at the end of the terminal
phalanges of the extremities, the hardened nail formations. The ridges
are due to the row-like arrangement of the papillae of the skin, some
times straight, slightly wavy, and crescentic; the crescentic are more pro
nounced in certain parts. In many regions the surface is divided up by
fine lines and furrows into many irregularly sized triangular, quadri
lateral, polygonal, elongated, and oval-shaped areas or spaces. The
larger furrows are much more pronounced about the joints, whereas the
smaller or surface lines are more noticeable on the extensor surfaces.
The pores—minute depressions—represent the orifices of the follicles
and glands of the skin. According to Philippson, some of the lines and
ridges, which might be termed ’‘primary,'’ are dependent upon prolifera
tion of the rete and linear depressions of the horny layer; and others
“secondary," or physiologic furrows, in the neighborhood of the articu
lations, resulting from the constant creasing induced by the incessant
joint motion. It is probable, too, that the distribution of the connec
tive-tissue fibers and bundles to which presumably are due the lines
of cleavage of Langer, may have an important and contributory bearing
on the production of these furrows and folds.
In a general way and in its gross features the skin can be divided
into two parts—the epidermis and the corium; commonly a third
division, of subcutaneous tissue, is added, but this last is in reality an
2 17
18 ANATOMY AND PHYSIOLOGY OF THE SKIN
extension or part of the corium, the natural connecting tissue that
joins the skin proper to the underlying body structures. Inasmuch,
however, as it is closely associated with the corium proper and often
contains the deeper glandular organs of the skin and the fat-cells, and as
many of the pathologic processes invade its substance, a knowledge
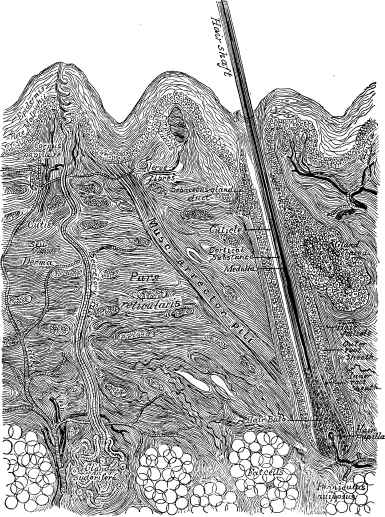
Fig. I.—Vertical section through the skin: general diagrammatic view (after Heitz-
mann).
of its anatomic structure and characters becomes a necessary part
of cutaneous histology. The epidermis is subdivided into several
layers. In addition to these parts the sebaceous glands, the sweat-
glands, the hairs, hair-follicles, and nails, commonly known as the
appendages of the skin, together with the blood-vessels, lymphatics,
nerves, and muscles connected with the integument and its nutrition
THE EPIDERMIS 19
and functions, are all to be considered as parts of its structure, and
are sometimes involved jointly or independently in its various morbid
processes.1
THE EPIDERMIS
The epidermis, also called the cuticle, cuticula, scarf-skin, or epi
thelial layer, is the outer or surface part of the skin, and is conveniently
divided into four layers—
the outermost layer, or
stratum corneum, known
as the horny layer; below
this an ill-defined, shin
ing layer, or stratum luci-
dum; and beneath this a
granular layer, or stratum
granulosum; and, finally,
the innermost layer, or
rete Malpighii, commonly
spoken of as the mucous
layer, rete, or Malpighian
layer. The outermost
part of the epidermis is
constituted of closely
packed cells, of horny
and dry character, the
cells becoming less dense
and less closely crowded,
and softer and even suc
culent as the lowest layer
of the rete is approached.
It varies considerably in
thickness in different parts
of the body, its thickest
development being ob
served on the palms and
soles, and its thinnest on
such parts as the eyelid,

Fig. 2.—Lines indicating cleavage of the skin
(Langer).
1 In the preparation of this section I am considerably indebted to Professor Duhr-
ing’s admirable description and judicial review, embodying the investigations of
Ranvier, Kölliker, Heitzmann, Robinson, Unna, Sappey, Bowen, and others contained
in his work, Cutaneous Medicine, Part I. Moreover, in order to combine terseness and
brevity with clearness in this description, I have frequently consulted and often bor
rowed expressions from the shorter and graphic contributions by Robinson, in his
Manual of Dermatology; by Louis Heitzmann, in Morrow’s System, vol. iii (Derma
tology); by Allen, in Twentieth Century Practice, vol. v (Diseases of the Skin); and by
Bowen, in Bangs-Hardaway’s American Text-Book. For a complete account of the
development of the chief cutaneous structures the articles “On the Development of
the Human Epidermis and Its Appendages,” by Macleod, in the British Journal of
Dermatology, beginning with 1898, p. 183, may be consulted, which, besides containing
much original work and many original illustrations, give a full and impartial presen
tation of the contributions of others; and which together with much other pertinent
matter is also to be found in his recent publication, Practical Handbook of the Pathology
of the Skin. See also a valuable but briefer account in Piersol’s Histology.
20 ANATOMY AND PHYSIOLOGY OF THE SKIN
the prepuce, etc, and due to different thicknesses of the corneous
layer, the rete remaining relatively uniform. It is developed from
the ectoderm. In earliest embryonic life this latter is primarily com
posed of but one layer of cells—epitrichial layer—below which several
rows of epithelial cells develop, the epi-
trichial layer finally disappearing toward
the sixth month of fetal life (Bowen).
Stratum Corneum.—The stratum
corneum, horny layer, or dead layer, is
the outer or surface division of the epi
dermis, and is composed of several layers
of flattened, imbricated epithelial cells
that have undergone various degrees of
keratinization, and that, in vertical sec
tion, appear spindle shaped, irregular, and
wrinkled. In the outermost layer these
cells have lost their cell characteristics
or appearance, and appear simply as
thin, flattened, dry scales. This appear
ance pervades to some extent the whole
thickness of the corneous layer, but is
less marked as the lower part is ap
proached, the cell character becoming
more and more recognizable, although
not conspicuously so, as the rete or liv
ing layer of the epidermis is reached.
In the lowest cells, with their sometimes
still visible polygonal outlines, a nucleus
is often faintly indicated. The outer
scales are being continuously cast off
during life, and are constantly renewed
by the lower layer of the epidermis, with
which it is histogenetically connected.
This layer can readily be called the dead
layer of the epidermis, as it gives no evi
dence of life, granular protoplasm being found, according to Unna,
only in the basal and superbasal layers.
Stratum Lucidum—The stratum lucidum, so designated by
Oehl, or translucent or shining layer, is a thin, ribbon-like, not always
well-defined layer, situated immediately below the stratum corneum,
of which it is considered by some to be a part. It is constituted of
closely set glistening or translucent epithelia, flattened and running
parallel with the surface, the separate cells not always being distin
guishable. According to Kaposi, this layer is supposed to be due to
some chemicobiologic change that the immediately underlying granular
or rete cells must undergo in order to become horny cells. It presents
no evidence of the granules of the subjacent layer, which have disap
peared presumably as a result of the peculiar change or in consequence
of the process of keratinization. According to Bowen, it is deeply

Fig. 3.—The epidermis: c,
Corneous (horny) layer; g,
granular layer; m, mucous layer
(rete Malpighii); the stratum
lucidum is the layer just above
the granular layer; d, corium.
Nerve terminations: n, Afferent
nerve; b, terminal nerve-bulbs;
l, cell of Langerhans (Ranvier).
THE EPIDERMIS
21
stained by certain reagents, especially those that have an affinity for
horny tissue.
Stratum Granulosum.—The stratum granulosum, as designated
by Langerhans, or the granular or hyaline layer, is next below the
stratum lucidum, and lies immediately upon the rete, of which it is
usually considered to be a part—the uppermost layer. It is composed
of one or two, rarely more, strata of coarsely granular, nucleated epi-
thelia. This granular material, composed of some peculiar chemical
substance, is, beyond the now generally accepted belief of its rela
tionship to the process of cornification, still a subject of discussion.
It takes the hematoxylin and picrocarmin or methyleosin stains well.
Ranvier, who considered it of partially fluid form, called it eleidin,
whereas Waldeyer named it keratohyalin, believing it to be of more
solid character and to resemble the nature of hyalin, and to be con
cerned in the process of keratinization. According to Buzzi, these are
two distinct substances: the first is fluid, and is found chiefly in the
lowest part of the horny layer, the second (keratohyalin) representing
the granules found in the cells of the stratum granulosum. On the other
hand, the granular material is thought by some to be a nitrogenous

Fig. 4.—Section of developing skin from human fetus of three and one-half months:
a, Layer of cuboidal cells representing rete mucosum; b, polyhedral elements forming
superficial layers; c, outermost flattened plates, probably the remains of the epitrichial
layer; d, mesodermic tissue forming corium (Piersol).
substance known as chitin, which is also found in the skin of insects and
in the shells of crustacea. The precise character and nature of these
granules cannot, therefore, as yet be considered as settled, Kromayer
even denying that they are concerned in the process of cornification.
Rete Malpighii.—The rete, rete mucosum, mucous layer, germ
layer, or Malpighian layer, as it is variously known, is an important
layer of the epidermis, and is concerned in most of the pathologic proc
esses of the skin. It lies immediately upon the papillary layer of the
corium, the granular layer forming its uppermost layer or boundary.
It is, therefore, the deepest stratum, and might be known as the living
stratum of the epidermis. In fact, as the studies of Carl Heitzmann and,
subsequently, Stricker indicate, the epithelia composing it together con
stitute a layer of reticulated protoplasmic living matter. It consists
of several strata of distinctly nucleated cells, irregularly polyhedral in
shape, especially in the upper part, rich in protoplasm, and arranged in
parallel rows. They readily take the carmin stain, as well as other
coloring-matters. The upper rows of cells, compared to those adjacent
to the corium, are somewhat broad and slightly flattened. The cells of
the lowermost part are columnar or cylindric in shape, with the nuclei
22 ANATOMY AND PHYSIOLOGY OF THE SKIN
correspondingly elongated, arranged in a palisade-like manner, and
with the lower broad or basal portion firmly fused with the papillary
layer of the corium by an interlacing of the projecting papillæ, and the
dipping-down elongations of the mucous layer. In addition, the cells
of the rete are furnished with radiating spines or prickles, and these
project into the corium and lock into one another; this interlocking,
together with the presence of a transparent albuminous substance or
cement that permeates the rete, makes this layer of the epidermis a
compact, resisting mass.
Owing to these prickles, spines, thorns, or spokes, the rete cells are
also known as " prickle-cells," and the layer as the " prickle layer” or
“thorny layer” of the epidermis. They are of the same structure as
the cells themselves, and result in a firm inter
lacing, becoming less prominent as the upper
most layer of the rete is approached. These
prickles have been thought to be canals for
the transference of fluid, but are now generally
considered to be simply outgrowths of proto
plasm, although it is not improbable that the
resulting interlacing channels left facilitate the
circulation of lymph and give space possibly
for nerve-threads, etc. It is in the lower cells
of the rete that the coloring-matter or pig
ment of the skin is found, varying in different
individuals and in different races, as will be
referred to further on. The so-called Herxheimer’s spiral fibers and
Langerhans’s cells remain to be described.
The Herxheimer’s “spiral fibers” or “epithelial fibers” are delicate
fibrils found at the basal portion of the rete, close to or at its junction
with the papillary layer of the corium, projecting upward parallel with
the columnar cells, usually in a spiral or tortuous manner, anastomos
ing with one another. They are made clearly definable only by special
methods of staining. Their origin and purpose are not clearly under
stood. Various opinions have been advanced: that they are canals for
the transference of nutritive material to the rete, projections of fibrin
from the corium, pigment-carrying wandering cells from the latter,
and epithelial fibers—the last being the more generally accepted view.
The cells of Langerhans are occasional cell-bodies found usually in the
deeper strata of the rete, and variously viewed as colorless tissue cor
puscles, wandering cells, lymphoid cells, and as pigment-cells deprived
or devoid of pigment. They are without nucleus, and are elongate and
irregularly stellate in shape.
CORIUM
The corium, or true skin, also known as the cutis, cutis vera, or
derma, is a development from the mesoblast; and, according to Unna,
even at birth the most superficial portion, which forms the foundation
of the subsequent papillary layer, consists of young granulation tissue
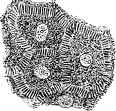
Fig. 5.—"Prickle-cells"
of the rete greatly magni
fied (Robinson).
CORIUM
23
with very few fibrillæ, whereas the cutis proper, or pars reticularis, has
at this time already acquired considerable thickness and density, in
consequence of the continuous deposition of collagenous substance
between its cells. It immediately underlies the row of columnar cells
of the rete, with which, by its papillary projections and the corresponding
interpapillary dippings of the rete and the prickles of the cells of the
latter, it makes a firm connection that is not readily disturbed. It is
composed of masses of fibrous and elastic tissue, especially the former,
which are closely intertwined, forming a dense and firm meshwork, most
compact at the uppermost part, becoming less so as the subcutaneous
tissue is approached. The bundles of anastomosing fibrous connective
tissue run parallel to the surface of the skin, and are arranged on a
definite plan, to which are due the lines of cleavage of the skin. They
are most numerous and in greatest abundance on those parts where
resistance and not elasticity is essential, as on the sole of the foot.
On the other hand, the elastic fibers are in greater number in regions
where motion and extensibility are necessary, as about the joints.
Compared to the amount of fibrous connective tissue, however, the
elastic tissue is relatively scanty, becoming more abundant with advanc
ing years. It is only during late years that the elastic fibers have received
much attention, more especially by Lustgarten, Unna, and C. J. White,1
this being rendered possible by means of new staining methods, the
ordinary methods not sufficing to make them visible. In addition to
these fibrous components, spindle-shaped connective-tissue corpuscles
or cells are seen here and there, and there is a cement-like substance
permeating the parts.
The corium constitutes the elastic and fibrous envelope of the body,
and contains blood-vessels, lymph-vessels, glandular structures, hairs,
fat-cells, muscle elements, and the nerves with their terminal organs of
touch and sensation. It varies in thickness on different parts, at differ
ent ages, and in different individuals; it is thickest over the palms, soles,
back, and buttocks, and thinnest on the eyelids and prepuce. It is
conveniently divided into two parts or layers—the papillary layer, or
pars papillaris, and the reticular layer, or pars reticularis, although it is
an arbitrary division, and one that is not sharply defined.
Pars Papillaris.—The pars papillaris, or papillary layer, is the
upper portion of the corium, which touches the rete above and extends
to just below the basal portion of the papillae. The papillary layer is
not an even or a level one, but is a wavy or zigzag line made so by
the innumerable glove-finger-like projections or upward prolongations
of the corium into the rete—the so-called papillæ. The rete layer fills
up the intervening gaps by corresponding downward juttings—the
interpapillary rete prolongations. The papillæ, composed of fine con
nective-tissue fibers running parallel to their long axis, vary considerably
in size, more especially in different regions, but even in the same place
there is often some variation. The largest, the so-called “compound
papillæ," are due to a bunching or an apparent fusing together of the
1 C. J. White, “The Elastic Tissue of the Skin,” Jour. Cutan. Dis., 1910, pp. 163,
217 (an elaborate paper, with bibliography).
24 ANATOMY AND PHYSIOLOGY OF THE SKIN
basal portions of several or more, the upper parts, of various length,
projecting like so many crowded fingers or like teats from an udder.
Probably most of them are, however, small conic or blunt protrusions.
They are arranged in rows, which may be straight, curved, or, as on the
finger-tips, concentric or crescentic, readily recognizable by the naked
eye. Their number is beyond computation: according to Sappey’s
calculation, there are about 150,000,000 over the entire surface, and
100 on a square millimeter. They are more numerous in some situations
than in others, and inasmuch as they contain the nerve terminals or
organs, they are found most abundantly on parts where sensitiveness or
the sense of touch is most acute, as on the terminal phalanges, penis,
clitoris, nipple, etc Some of the papillae contain loops of blood-vessels
—vascular papillæ; others, the nerve terminals or organs—nervous
papillae. The latter have, as a rule, only a limited vascularity, but some
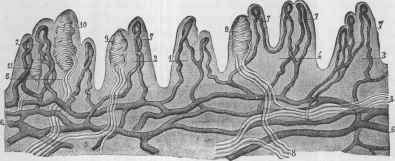
Fig. 6.—Section of palm of hand showing single and compound papillæ and their
blood-vessels, with terminal vascular loops: 1, 2, 3, 4, 5, Compound papillæ, contain
ing one or more vascular loops; 6, 6, network of blood-vessels; 7, 7, 7, 7, 7, vascular
loops; 8, 8, 8, beginning subpapillary nerve-plexus; 9, 9, and 10, 11, tactile corpuscles
with from two to four nerve-fibers (Sappey).
papillae contain both nerve-endings and vascular loops, especially the
compound papillæ.
Pars Reticularis.—The papillary layer passes imperceptibly
into the reticular layer, this latter merging into the subcutaneous tissue
beneath. It is of looser texture than the pars papillaris, and the bundles
of connective-tissue fibers are larger and coarser. The fasciculi, espe
cially in the lower part, have a more oblique direction. It has received
the name reticular layer from its reticulated appearance. It consti
tutes the bulk of the corium. It contains some of the glandular struc
tures, hair-roots, and muscles, and, like the papillary layer, is liberally
supplied with blood-vessels, etc
SUBCUTANEOUS TISSUE
The subcutaneous tissue, or hypoderm, as it is designated by Besnier,
immediately underlies the reticular layer of the corium, and probably,
as Unna states, owes its recognition as a distinct layer “only to the
circumstance that, in consequence of the macroscopically appreciable
BLOOD-VESSELS
25
deposit of fat in it, a distinct borderline is visible even to the naked eye.”
The division is, however, usually considered higher up than the layer
of fat-cells, although most authors agree that it is a purely arbitrary
one, with no sharp or appreciable boundary-line.
Like the corium, the subcutaneous tissue is composed of a network
of interlacing and anastomosing fasciculi and bundles of connective
tissue, less densely arranged than those in the corium, and inclosing irreg
ular and rhomboidal spaces containing the masses of fat-cells. Lym-
phoid corpuscles are present in this layer, especially in the neighborhood
of the blood-vessels and glands. It is essentially a continuation of the
reticular layer, so far as its connective-tissue formation is concerned,
with looser meshes, and gradually disappears into and is attached to the
fasciae and aponeuroses of the muscles and the deeper structures beneath.
The roundness and fulness of the integumental covering are due
to the presence of the masses of fat-cells contained within its interstices,
and should they disappear by absorption or depletion in consequence
of starvation, fever, or emaciating disease, a looseness or wrinkling
results.
The fat-globules are spheric vesicles consisting of an elastic capsule,
with an oval nucleus at one point, and a drop of oil filling the cavity.
They are grouped in a lobular manner, and are separated from one
another by delicate fibrous connective tissue with a comparatively
abundant supply of blood-vessels having an afferent artery, one or two
efferent veins, and a capillary plexus (Louis Heitzmann). Owing to
the abundance of the fat-cells present this structure is designated
panniculus adiposus, stratum adiposum, or adipose tissue. Warren’s
studies showed, especially where the cutis is thick, fat columns (columnæ
adiposæ) projecting from the subcutaneous tissue obliquely upward
through the corium to the bulb of the smaller hairs, and some containing
a coil-gland that they help to support, their axes being parallel with the
arrectores pilorum. The fat-globules are absent in certain regions, as on
the eyelid, in the auricles, on the penis, scrotum, and labia minora. The
subcutaneous tissue contains the sweat-gland coils, the deeper-lying
hair-follicles, trunks of blood and lymph-vessels, nerves, corpuscles
of Vater, and the Pacinian bodies.
BLOOD-VESSELS
Both the corium and the subcutaneous tissue are highly vascular
and liberally supplied with truncal and capillary vessels. The epi
dermis has no vascular supply. Two horizontal and parallel plexuses
are to be seen—a deep and coarser one, in the subcutaneous tissue, and
a fine, delicate, and minutely ramifying layer just beneath the papillae,
and loops from this system extending up into the latter. In some of the
papillæ the loops are quite well defined, but in those containing the
developed nervous structures the vascular supply is not so clearly
recognizable, some, according to Robinson, frequently having no blood-
vessels, although Thin believed that the nervous papillæ contained loops,
these being of an extremely fine and delicate character. This upper
26 ANATOMY AND PHYSIOLOGY OF THE SKIN
plexus is connected with the lower vascular network by numerous large
truncal vessels. The vessels forming this lower plexus consist of fairly
large arterial and venous channels, from which ramifications extend
to the coil-glands and to the fat-cells. The coil-glands are liberally
supplied, being more or less surrounded by a delicate plexus of arterioles
that empty into two or three small veins, one of which always follows
the duct upward, finally anastomosing with the veins of the papillary
layer. The sebaceous glands and hair-follicles are likewise abundantly
supplied, the hair papilla having its own arteriole branching into looped
capillaries; transversely arranged capillaries are found between the layers
of the follicles, which also penetrate their inner sheath, and the venous
plexuses accompany the arterial in all parts, the venous vessels being
usually somewhat larger than the arterial.
According to Tomsa, as cited by Louis Heitzmann, the skin has
three distinct vascular districts, each of which is supplied with its own
arterioles and roots of veins; the deepest is that of the subcutaneous
fatty tissue, the middle that supplying the sweat-glands, and the upper
most belonging to the derma with its hair-follicles and sebaceous glands.
LYMPHATICS
Lymphatic vessels are abundantly supplied to the integumentary
tissues, and have been studied especially by Sappey, Biesiadecki,
Neumann, Klein, and a few others. They are found forming numer
ous plexuses (Klein), but more particularly a superficial and a deep
network. The former is just below the superficial plexus of blood-
vessels, and consists of minute ramules, from which blind shoots or
short loops extend into the larger papillæ. Intercellular lymph-spaces
are to be found in the epithelial layer of the epidermis, and seem, from
injection demonstrations, to be in some manner connected with the
lymphatic system of the derma. Indeed, lymph-channels and spaces
without independent walls exist in all parts of the skin (Neumann,
Unna, and others), and especially in the interstices of the fibrous tissue
of the corium, and, although a part of the lymphatic system, their rela
tion to the lymphatic vessels is still not known definitely. Klein believes
that the lymphatics have open communication, by true stomata, with
these spaces, which he looks upon as lymph-rootlets. The deeper plexus
of lymphatics is situated close to the subcutaneous network of blood-
vessels; in fact, blood-vessels and lymphatics are found for the most
part accompanying one another (Louis Heitzmann). The superficial
and deeper layers, as well as other lymphatics, are joined by anastomos
ing branches. Many of the larger vessels have valves and corresponding
constrictions. According to Neumann, the hair-follicles, as well as the
sebaceous and sweat-glands, have their own system of lymphatic capil
laries, and Klein likewise divides them into several systems, correspond
ing to these parts and also to the connective-tissue matrix and the adi
pose tissue.
NERVES
27
NERVES
The skin is well endowed with both medullated and non-medul-
lated sensory nerve-fibers, the former sometimes losing their sheath
and continuing as non-medullated fibers. They are found often in com
bination. The medullated are most abundant where the Pacinian and
tactile corpuscles are numerous. They arise from nerve-bundles that
are found spread out in the form of plexuses corresponding to the sub-
papillary and subcutaneous vascular network.
The glands, blood-vessels, and Pacinian corpuscles are supplied from
the nerve-bundles in the subcutaneous tissue and lower corium—
from the lower plexus. These bundles pass upward, the fibers spread
ing out and running horizontally, and forming a subpapillary plexus
consisting of a close and fine network of non-medullated fibers. Within
the papillæ, around the capillaries, they form a dense plexus of thick
or fine varicose fibers with many nuclei (Robinson). From this plexus,
again quoting Robinson, non-medullated fibers pass toward the epi
dermis and enter it either directly or after running a short distance
parallel to its surface. Penetrating the rete, they lie between the epi
thelial bodies and form a plexus. Langerhans believes that they anas
tomose between the cells and end in minute swellings or club-shaped
extremities, whereas, according to Unna’s observations, the final distri
bution is intracellular, each cell containing a pair of nerve-endings.
The nerve-fibers do not all, however, terminate in this way, for
many, as previously stated,—and this concerns especially the medul-
lated nerves,—end in the Pacinian corpuscle, whereas some of those
projecting upward to the surface terminate in the tactile corpuscles
of the papillæ—the so-called corpuscles of Meissner or Wagner, and
of Krause—and in Merkel’s touch-cells. A large number of the medul-
lated fibers, however, pass upward to the papillæ, where they form loops
and return to the subpapillary region, and several of these looped medul-
lated fibers are sometimes present in a single papilla (Robinson).
The exact or relative purpose and function of these various bodies
are not fully known, except that it is generally agreed that they are
sensory organs. According to Merkel, cited by Duhring, the tactile
corpuscles and the touch-cells are organs for the finer perceptions, and
the bulb-corpuscles and Pacinian bodies for localization and common
sensation; the free nerve-endings in the epidermis may subserve touch
as well as temperature, and those in the hair, both touch and sensation.
Pacinian Corpuscles.—The Pacinian corpuscles, also known
as the corpuscles of Vater, are most numerous in the subcutaneous
tissue of the last phalanges of the fingers and toes and the palms and
soles. They are also abundantly met with on the nerves of the joints
(Duhring). As many as 95 have been found upon the index-finger, and
608 on the entire hand (Herbst). Their function is not clearly under
stood, but, as Bowen states, their situation in parts especially sensitive
indicates some connection with the tactile sense, although this view is
seemingly opposed by their deep position. They are clearly defined, oval,
elliptic, or pear-shaped grayish bodies, made up of concentrically arranged
28 ANATOMY AND PHYSIOLOGY OF THE SKIN
capsules—20 to 60, according to Kölliker—with an elongated central
clear space containing a transparent matrix and limiting membrane and
inclosing a stalk-like nerve terminal—the ending of a medullated nerve-
fiber that enters at the lower extremity of the corpuscle.
The various concentric layers are separated by septa into smaller
and larger spaces, containing a clear serous fluid, and lined with a
single layer of epithelium; they are composed of connective-tissue fibers
and connective-tissue corpuscles. The fibers are arranged in a longi
tudinal layer, especially toward the inner portion, and in a circular layer
toward the outer portion; these two layers are, according to Ranvier,
connected or crossed by transverse or “radial” fibers. The medullary
sheath and sheath of Schwann cease at the entrance of the nerve into the
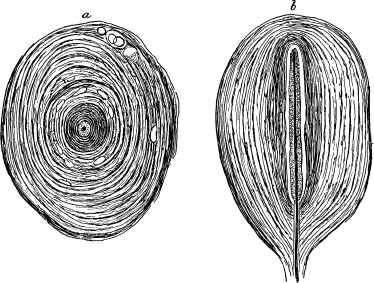
Fig. 7.—Pacinian corpuscles from the derma of the palm of the hand; stained with
aurum chlorid (X 500): a, Transverse section; b, longitudinal section (Louis Heitz-
mann).
central clear space (Robinson). Unna considers the corpuscle due to an
enormous enlargement of the latter sheath into concentric lamellæ, with
nuclei and endothelial lining.
Tactile Corpuscles.—The tactile or touch-corpuscles, also
known as the corpuscles of Meissner or of Wagner, are ovoid or round
ish fibrous bodies found in the papillæ, occupying the greater portion
and sometimes the entire extent, and usually those papillæ that have
no vascular loop. Occasionally they are found somewhat beneath, in
the papillary layer. They are exceedingly numerous, varying in number
on different parts, being most abundant on the ûngers, especially the last
phalanges, where, according to Meissner, one papilla in every four con
tains a tactile corpuscle. Occasionally two, rarely three, are found in one
papilla, although in some instances, according to Robinson, one corpuscle
NERVES
29
has the semblance of two, this resulting from a constriction caused by the
nerve. They are well defined, with transverse bands or striations, and
small nuclei (Bowen), the mass of the body consisting of nucleated con
nective tissue (Langerhans, Thin), although their exact structure is in
volved in some uncertainty. One or
two medullated nerves, ascending
from the corium, enter the corpuscle
at its extremity or side, their myelin
sheath being lost in the fibrous mass
of the capsule; dividing into delicate
fibrillæ, they wind spirally in a vari
able course along and through its
structure, anastomosing with one an
other, their termination being a mat
ter of some doubt—in a number of
terminal fibrils (Bowen), in slight
pear-shaped or cylindric enlarge
ments (Louis Heitzmann), or, after a
greater or lesser number of wind
ings, leave the corpuscle at its apex
as one, sometimes as two, efferent
fibers (Robinson). In fact, accord
ing to Robinson, each corpuscle has
an afferent and an efferent nerve.
Corpuscles of Krause,
bulb-corpuscles, or end-
bulbs, originally described and
designated by Kölliker as “papillæ
fungiformes,” and regarded by him
as undeveloped touch-corpuscles, re
semble the inner structure of the
Pacinian body, and seem to be the
terminal corpuscle of some of the
medullated nerves coming from the
deeper plexus. They vary somewhat
in form between this and that of the
tactile corpuscle, although Krause
believes that they possess features
that serve to distinguish them.
They are observed especially about the sensory mucous membrane—the
vermilion of the lips, the tongue, the conjunctiva, the glans penis, and
the clitoris; in the two last-named regions they are larger and mul
berry shaped, and lie deeply under the papillæ—the genital nerve-
corpuscles of Krause.
Merkel's Touch-cells.—Merkel has described minutely a touch-
cell in which a medullated nerve terminates, situated in the epidermis
and superficial corium. These touch-cells have since been studied
by Kölliker and Ranvier. They are ovoid in shape, with a nucleus
and nucleolus, and are found in regions where tactile corpuscles are

Fig. 8.—Tactile corpuscle from
finger-end, treated with osmium,
showing the two afferent nerves (pur
posely accentuated), disappearing in
the upper part. The transverse nuclei
belong to the neurilemma of the
nerve-fibers (after Kölliker).
30 ANATOMY AND PHYSIOLOGY OF THE SKIN
few in number, as upon the abdominal surface. According to Kölli-
ker’s observations, they are numerous also on the finger-tips and plantar
surface. There is still considerable diversity of opinion both as to their
nature and their function.
Vasomotor and Motor Nerves.—The sensory nerves are not
the only nerves of the skin, as, according to Kölliker, cited by Duhring,
motor nerves are found on the smooth muscles and on all glands that
have a muscular layer. The vasomotor nerves also probably play
an important rôle, but although they are often spoken of in discussing
the pathology of diseases, but little in reality is known concerning them.
The general belief is that they probably exist in two varieties, those
having connection or association with the central nervous system, and
those connected with the ganglionic plexuses adjacent to the integument
itself. Being particularly abundant around the cutaneous arterioles,
it can readily be seen how they can, by increase or diminution of the
circulation, and by dilatation or tension, exercise a marked influence
upon the vascular, muscular, and glandular systems of the integument.
The well-known occurrence of flushing and blanching of the skin,
the “cold sweat’’ in sudden nervous perturbation, the production of
“goose-flesh,” etc, all point to the possibly profound pathologic
action that emotional, toxinic, or other disturbance of these nerves
may excite.
MUSCLES
The skin is supplied with both striated and smooth muscles, the
latter being much more abundant than the former.
The Striated muscles are found chiefly in certain regions, as
on the face and neck, and arise from the subcutaneous tissue and deeper-
seated muscles, and extending upward vertically or obliquely between
the glands into the corium.
The non-striated or smooth muscles are very numerous,
and run obliquely or parallel to the general surface; if the latter, they
run either in a straight or in a circular direction. The straight muscles
anastomose with one another and form a network or plexus, as in the
scrotum,—constituting the tunica dartos,—prepuce, and perineum;
those running circularly form a ring-like muscle, as in the areola of the
nipple. According to Unna, fasciculi arranged in strata, and lying
almost perpendicularly to the direction of cleavage, are found in the
corium. The majority of the obliquely running muscles are connected
with the hair-follicles and sebaceous glands, although they are also
observed, according to Tomsa, Unna, and others, in many regions, as
on the forehead, the cheeks, the back, etc, independently of these
structures.
The follicular muscles—the arrectores or erectores pilorum
—extend from their point of origin in the inner sheath of the follicle
obliquely upward, close to the lower surface of the sebaceous gland,
to the papillary layer of the corium. In its course upward it frequently
divides into two or more bundles, these secondary bundles afterward
PIGMENT
31
pursuing different directions, or uniting with fibers from other muscles
and forming a network in the corium; occasionally several secondary
bundles run nearly parallel to one another, and terminate either sepa
rately or conjointly (Robinson). According to Klein, Unna, Nékam,
Balzer, and others, they have an abundance of traversing and surround
ing elastic fibers, and terminate in veritable tendons of similar elastic
tissue. It is probable that the muscular and elastic fibers together play
an important part in influencing and regulating circulatory and glandular
action. The arrector muscles are of general distribution; they are seen
most completely developed and in greatest abundance in the scalp, on
the mons veneris, and on the scrotum, whereas in certain hairy regions,
according to Kölliker, as in connection with the hairs of the eyelashes,
eyebrows, and the axillae, they are wanting. The erectile condition
known as “goose-flesh,” or cutis anserina, is produced by the sudden
contraction of these muscles over the general surface. Overlying the
sebaceous glands as they do, their contraction naturally tends to com
press and evacuate these structures, this probably being an important
part of their function.
PIGMENT
The pigmentation of the skin has its chief seat in the lower strata
of the rete, appearing as a darkened stratum above the papillary layer
of the corium. It is due to a faint staining of the cells themselves,
most pronounced in the nuclei, and to the deposition of fine granules
of pigment—melanin—in the cell cavity. The resulting color of the
skin is naturally considerably influenced or modified by the degree of
vascularity. Unna is strongly of the opinion that the color of the white
race is due largely to the presence of the granular layer, whereas Kro-
mayer, as cited by Duhring, attributes it to several conjoint factors—
principally to translucency of the epidermis and corium, the anemic
condition of the papillary layers, and the presence of fat in the subcu
taneous connective tissue. In the dark-skinned races the quantity of
pigment deposit is markedly greater, varying according to the degree of
coloration of the skin. The pigment-cells are more highly colored, and
staining involves the whole rete and upper corium, and usually extends
to some degree to the cells of the horny layer. The pigment granules
are much darker, and occur in greater abundance than in the white race.
The children of dark-skinned races are usually born apparently white,
or relatively so, coloration then taking place rapidly. Morison’s investi
gations as to the negro skin show, however, that beginning pigment de
posits are found several weeks or more before birth. Thomson, cited by
Macleod, detected pigment granules in the skin of a negro fetus as early
as the fifth month, forming a yellow stain in the deeper cells of the
prickle-cell layer. According to Karg, white skin transplanted upon the
negro becomes pigmented, and the color of the negro skin transferred
to the white man soon disappears.
The origin of the pigment is involved in some uncertainty. Various
views are held, among them being the following: That it is carried up
32 ANATOMY AND PHYSIOLOGY OF THE SKIN
by the leukocytes from the underlying subcutaneous tissue (Bichat,
Riehl, Aeby, and Ehrmann), that it is due to the migration of the pig-
mented cells of the adjacent connective tissue (Kölliker); or that it is
formed within the protoplasm of the cells in loco, the earliest pigment
appearing within mesoblastic cells that have entered the epidermis while
still uncolored (Piersol). Unna considers that the pigment is formed
from the coloring-matter of the blood, and is carried up to the epidermis
by “chromatophores” or “wandering cells,” a view practically shared by
List. Macleod thinks it probable that the “chromatophores” are
lymph-cells, and that the pigment formed from the blood in the cutis is
carried in the lymph-stream to the inter epithelial spaces, and reaches

Fig. 9.—Section of negro skin, including epidermis (a) and papillary layer (b)
of the corium. The pigment is contained in the deepest layer (c) of the epidermis
(Piersol).
the nuclear region of the cells by passing along the tracks of the nerve-
fibers. Both Meirowsky and Dyson consider that the epidermis pro
duces its own pigment,1 Meirowsky’s investigations showing that pig
ment is of autochthonous origin, probably produced by the action of
a ferment on the protein molecule of the cell. Dyson2 believes that it
is a lipochrome in origin, the melanin being the chromatic protein por
tion after its separation from the complex lipoid granules, and that it
is a product of the nucleus.
1 McDonagh, Brit. Jour. Derm., 1910, p. 316, gives a good review of the pigment
question to date.
2 Dyson, “Cutaneous Pigmentation,” ibid., 1911, p. 205 (with illustrations and
good review to date, with bibliography).
SWEAT-GLANDS 33
SWEAT-GLANDS
The sweat- or coil-glands, also known as sudoriparous glands,
glandulæ sudoriferæ, glandulæ glomiformes, are seated in the subcu
taneous tissue and in the lowermost part of the reticular layer of the
corium. They consist of a simple tubule
coiled upon itself, forming an ovoid or
globular convoluted body with a blind
end in the central or outer part of the
coil, and the excretory duct. This lat
ter is essentially a continuation of the
tubule somewhat altered, beginning
usually in the middle or upper central
portion of the mass, and traversing the
corium directly and generally straight
upward and between the papillae, its
course becoming somewhat less regular
in the rete, and passing through the
corneous layer in a peculiar wavy, spiral,
or cork-screw manner, and opening upon
the surface in a rounded, funnel-shaped
aperture—the so-called sweat-pore.
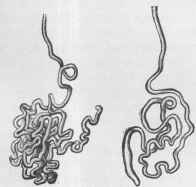
Fig. 10.—Sweat-glands of different size (of
moderate magnification) showing coil or convo
lutions forming gland proper, the blind end of
tubule, and excretory duct (Sappey).

Fig. 11.—Section through
sweat-gland, duct, and outlet (of
greater magnification): a, Coils
forming gland; b, beginning of ex
cretory duct; d, excretory duct; e,
sweat-pore; f, corneous layer; g,
stratum lucidum; h, granular layer
(von Brunn).
The coil or gland proper is the secreting part of the tubule, and con
sists of a lining of secreting cuboidal or polygonal, somewhat granular-
looking epithelia, of a basement or investing membrane made up of
flattened endothelial cells and, between the latter and the layer of secret
ing cells, some unstriped muscular fibers. A layer of such fibers is also
found in certain glands, especially those of the axillæ, external to the
investing membrane (Robinson). Virchow states that the covering
membrane is made up of connective-tissue fibers and connective-tissue
nucleated cells, running longitudinally with the canal, the inner portion
representing the membrana propria.
3
34
ANATOMY AND PHYSIOLOGY OF THE SKIN
The secreting epithelial layer is made up of a single layer of cells,
with nuclei and one or two nucleoli, and, according to Heynold, their
inner surface shows a delicate limiting membrane, especially defined
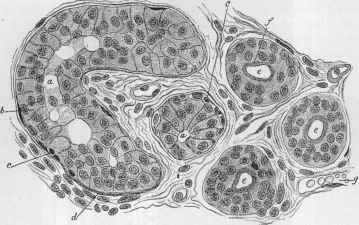
Fig. 12.—Section through a sweat-gland (X about 400): a, a, Secreting part of coil;
b, gland-cells; c, smooth muscle-fibers; d, membrana propria of the duct; e, e, e, cross-
cut of duct; f, cuticular lining of duct; g, blood-vessel (Rabl).
in the larger glands. There is a well-marked lumen in which, as well
as in the cell-body, oil-globules are usually present. The glandular
structure is embedded in considerable, but somewhat loose, fibrous con
nective tissue, which is denser and
contains a larger number of lym-
phoid cells between the tube-coils.
The vascular supply is abundant,
the blood-vessels from the deep
plexus surrounding the coils like a
network, with numerous vessels
penetrating between the coils.
Ranvier has shown also the exist
ence of an inclosing network of
nerve-fibers, some of which pene
trate through the investing mem
brane to the muscular layer.
The excretory duct presents a
somewhat different structure from
that of the coil. As the duct ex
tends upward there is an increase
in the number of epithelial cells,
these forming a double layer and
gradually showing a distinct lining
or cuticular covering. The duct loses its investing membrane and
muscle-fibers when it enters the rete, and, in this region, eleidin granules
have been observed in the cells. In the stratum corneum the duct-wall
is formed of cells of this layer.
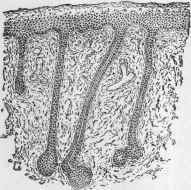
Fig. 13.—Section of skin of human
fetus, showing developing sweat-glands.
The latter grow as epithelial cylinders
from the rete mucosum of the epidermis
into the underlying corium; the character
istic coil appears later (Piersol).
SEBACEOUS GLANDS
35
The first recognizable signs of the development of the sweat-glands
are observed in the fifth month of fetal life, and consist of an ingrowing
or budding of the rete cells in the form of conic epithelial processes into
the corium. By the sixth month elongation has taken place, and from
that time on the coil-formation gradually progresses; in the seventh
month the canal appears, and the lower end of the tube is observed to
be dilated and somewhat twisted; by the ninth month the tube is coiled
upon itself and the gland proper is formed (Robinson). Their distribu
tion is extensive and general, although Klein and Robinson failed to find
them on the margin of the lips and on the glans penis. Their number is
extremely large—estimated to be, for the entire surface, slightly over
2,000,000 (Krause, Sappey). They are most numerous on the palms
and soles, where, according to Krause, from 2600 to 2700 exist in a square
inch. They vary somewhat in size in different situations, being largest
in the axilla and in the anal region. The larger coils sometimes show
irregularly distributed constrictions and dilatations, and, according to
Kölliker, the tubules of some of the large glands of the axilla exhibit a
number of fork-shaped branching sacs.
SEBACEOUS GLANDS
The sebaceous glands, known also as oil-glands, glandulæ sebaceæ,
glandulæ sebiferæ, and hair-follicle glands, are racemose or acinous
glands usually connected with or in close relation to the hair-follicle,
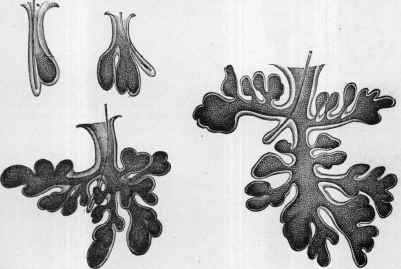
Fig. 14.—Sebaceous glands of the face—simple pouch to compound lobular, with lanugo
hair and small or rudimentary hair-follicle, the largest from the nose (Sappey).
and seated in the corium. They are also observed in regions where there
are no hairs, as on the glans penis, inner surface of the prepuce, labia
minora, and red border of the lips. Unna would designate the glands
36 ANATOMY AND PHYSIOLOGY OF THE SKIN
of these several regions as the “sebaceous glands of the mucous orifices.”
They are, therefore, to be found upon almost all parts, although they
are absent on the palms, soles, and dorsum of the third phalanges.
In connection with large hairs the gland is essentially an appendage of
the hair-follicle, into which it empties; this is especially shown with the
scalp-hairs. With small lanugo hairs, on the contrary, the reverse ap
pears to be the case, the glandular structure and duct being relatively
much larger than the hair and follicle, as conspicuously noticeable in
the nose-glands. The largest are found upon the nose, especially at the
labionasal fold, the cheeks, eyelids (Meibomian glands), the areola
of the nipple, the mons veneris, the labia majora, the scrotum, and
about the anus. The glands found upon the penis and inner surface of
the prepuce—Tysonian glands, unconnected with hair and opening

Fig. 15.—Model of sebaceous
gland group of a scalp hair: a,
Hair-follicle; b, lobulated gland;
c, tubular gland; d, alveolar
gland (Bauer).
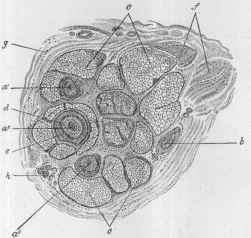
Fig. 16.—Cross-section of skin of scalp on a
level with the sebaceous glands: a1, a2, a3, Hairs;
c, c, sebaceous glands; d, inner root-sheath; e,
outer root-sheath; f, arrector pili; g, connective
tissue; h, sweat-gland (X 30) (Rabl).
upon the free surface—vary in development, and are somewhat incon
stant, sparse, or numerous.
Although fundamentally the same in structure, sebaceous glands
vary considerably in size and form. The simplest is a mere small pouch-
like body, and various forms from this up to one distinctly multilobular
and racemose are to be seen, as shown in the accompanying cuts.
The gland-structure consists of a secretory portion and duct, the
latter emptying between the surface of the hair and the inner root-
sheath of the latter. The hyaline basement membrane of the gland
is surrounded by dense connective tissue arising from the hair-follicle
or from the corium, and containing blood-vessels, nerves, and lym
phatics. Upon the basement membrane are seated several layers of
epithelial cells, the outermost resembling those of the rete. In this
layer the cells are cylindric and columnar; toward the inner portion
THE HAIR
37
they become larger and more or less cuboid or polyhedral, and con
tain fat-globules, the fatty degeneration of the cells taking place in
the center of the cells; this is most noticeable in the cells of the inner
most layer. The various lobules or acini empty into a common gland
cavity, which is observed to contain fat-globules, fat crystals, and
epithelial débris, and this finds final exit through the excretory duct,
which is also lined with epithelial cells, into the hair-follicle, or, where
there are lanugo hairs, often more or less directly upon the free surface
of the skin. The glandular product, together with the epithelial débris
from the excretory duct, constitutes what is known as sebum or sebaceous
matter. The so-called smegma, formed about the glans penis and inner
side of the prepuce, is not at present believed to be the product of the
sebaceous glands, but to be due chiefly to an exfoliation of the horny
layer of the epidermis. It is not improbable, however, that both may
be factors in its production. Not uncommonly a parasitic mite, the
acarus, or demodex folliculorum, generally considered to be harmless, is
found in the sebaceous gland, especially its duct, with its head usually
toward the gland.
The first sign of the development of the sebaceous glands is usually
noticed in the third or the fourth month of fetal life, and appears as a
budding from the external root-sheath of the hair-follicle; primarily
they consist of epithelial cells that, by multiplication and further pro
jection downward, form the gland. They have a rich vascular supply,
and are surrounded by a network of capillaries. Like the hairs, they
appear first in the skin of the eyebrows and forehead, and spread over
the trunk to reach the extremities last (Macleod).
THE HAIR
Hairs are short or long, rounded or cylindric, horny formations
derived from the epidermis, having their seat in obliquely directed
pouch-like depressions in the corium, commonly known as the hair-
follicles or hair-sacs. As a rule, but one hair is implanted in each follicle,
but exceptionally two and even three hairs have been observed.
The hair varies considerably in different individuals, and especially in
those of distinct nationality or type, the differences being due mainly
to the degree of straightness or curl, caliber, length, and color (Duhr-
ing). The negro hair-follicle and its contained portion of the hair-shaft,
according to the studies of Browne, C. Stewart, and Anderson Stuart,
are much longer than in the white, and are remarkably curved, this
latter feature, Anderson Stuart suggests, accounting for the curl in the
projecting shaft. The hairs are very abundant, but their number varies
considerably. On the scalp of average growth there are about 1000 to
the square inch, approximately 120,000 to the entire region (E. Wilson).
The hair of lightest color always shows the greatest number (140,000),
whereas red hair is least abundant (90,000), the brown (109,000), and
the black (108,000) occupying a middle position between these two
extremes (Duhring). Owing to the direction of the obliquely set fol
licles, which bears some relation to the various planes of the surface, the
38 ANATOMY AND PHYSIOLOGY OF THE SKIN
hair-growth has various centers, and, as Eschricht has shown, exhibits
in the arrangement of both the short and long hairs, curves and
whorls.
Hairs are found in all regions except the palms, soles, backs of the
last phalanges of the fingers and toes, lips, glans penis, and inner surface
of the prepuce. They may be divided into three forms: (1) Lanugo,
or fleecy or downy hairs, which are short, soft, and extremely fine, as
with those usually seen upon the face, trunk, buttocks, and limbs; (2)
short, strong, or bristly hairs, somewhat thick, such as the eyelashes,
the eyebrows, and those in the nares and in the outer auditory canal;
(3) long hairs, of variable length from a few inches upward, and exempli
fied by the hairs of the scalp, beard, axillæ, and genital region.
Two parts of a hair are usually distinguished—the hair-shaft, or
that portion exterior to the skin, and the hair-root, or that contained
within the follicle. The hair-root is thicker than the shaft proper,
and becomes more markedly so at its lower part, where it expands
into a bulb-shaped body, known as the hair-bulb, which is seated upon
and grasps the hair papilla. Both in
its shaft and root a hair consists of an
outer thin covering or cuticle, a cortical
mass, and usually a medullary portion,
or medulla.
The cuticle is a transparent mem
brane enveloping the whole hair, and
composed of thin, non-nucleated imbri
cated lamellæ arranged in an overlap
ping fish-scale and shingle-like manner,
with the free or outer portion, slightly
elevated and pointing toward the distal
end of the hair, giving it a serrated or
reticulated appearance. The cortical
substance or mass, or main body of the
hair, is made up of delicate flat, fusi
form, nucleated, firmly attached epi
dermal scales, which are so closely fused
or agglutinated as to form narrow,
elongated, spindle-shaped bundles of
fibers; they show longitudinal striations, are more or less uniformly
colored, and often contain, both within and between the scales, a vary
ing amount of pigment-granules and diffuse pigment. The medulla, or
medullary portion, in the center of the shaft, is not present in all hairs,
being usually absent in lanugo, and most clearly shown, as a rule, in thick,
short, and strong hairs. It extends from the bulb almost to the free
end, often uniformly as a cord-like structure; sometimes, however, it is
somewhat irregular or broken. It consists of epidermal elements, often
pigmented, and frequently showing granules that were formerly thought
to be pigment-granules and fat, but that, according to recent investiga
tions, are now believed to be, in great part at least, air-vesicles.
The hair-root, or the part of the hair implanted in the skin, or within
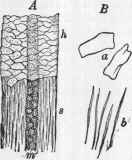
Fig. 17.—A, Human hair: the
upper half of the figure represents
the superficial horny cells (h) con
stituting the cuticle; the lower half
(s), the fibrous structure of the cor
tical substance and m, the medulla.
B, isolated elements of the hair: a,
Cuticular scales; b, thin fiber-cells
of cortical substance (Piersol).
THE HAIR
39
the hair-follicle, is, in its upper part, structurally the same as the out
lying shaft. Toward the lower portion, or hair-bulb, however, the
fiber-like character gradually disappears, the lamellae becoming softer,
and changing into spindle-shaped nucleated cells. Further down they
are polyhedral in shape, and the lowermost, those about the hair papilla,
are cylindric. These cells resemble closely those of the rete, and often
contain pigment-granules—so many, in some instances, as to constitute
true pigment-cells.
In the deepest portion of the hair-bulb are found a variable number
of stellate pigment-cells that are, presumably, as believed by Kölliker,
Aeby, and Riehl (cited by Duhring), wandering connective-tissue cells
from the hair papilla, and of importance in the function of pigment-
formation.
The hair-bulb lies within either the corium or upper subcutaneous
tissue, the lower part, in the stronger hairs, not infrequently extending
into the latter. It is a club-shaped expansion, seated upon and embrac
ing the hair papilla. It is surrounded by the inner root-sheath, or root-
sheath proper, of the hair-follicle, which extends upward to the duct of
the sebaceous gland. In transverse section the hair is of rounded or ellip
tic form, the latter being most pronounced in markedly curly hair, and
least so in straight hair.
The color of the hair is due mainly to the varying amount of pigment-
granules and diffuse pigment present in the cortex, or body of the hair,
and the medullary portion. The presence of air, usually as air-vesicles,
is also, doubtless, an important factor, especially in contributing toward
light blonde, white, or gray hair. Indeed, according to Pincus, the
presence of air in the cortical substance or in its outer portion may give
the hair a whitish or grayish color, even though the central part be
distinctly dark. It is presumably owing to a rapid evolution of air-
vesicles that “sudden graying of the hair” (q. v.) is produced.
The first sign of the development of the hair is observed usually
at the end of the third fetal month, and consists of a downward, cone-
like or club-shaped projection of the rete, covered with the horny layer.
According to Unna, this is first observed on the face, and not until
toward the seventh or the eighth month on other parts. Macleod states
that the earliest development is noted on the forehead and eyebrows, be
tween the second and the third month, and on the back, breast, and
abdomen, about the fourth month, reaching the dorsal aspects of the
hands and feet between the sixth and the seventh month. This rudi
mentary formation is gradually surrounded by connective-tissue cells,
extends more deeply, expands at its lower end, and grasps the papilla,
which, in the mean time, has arisen from the corium. The young hair
continues to grow, and after a time—about the end of the fifth month—
its pointed tip perforates the cone, through the horny layer, and the hair
becomes exposed. The embryonal or early hairs are always of the
lanugo type, and devoid of medullary substance, having a small and
short follicle, and usually a relatively large sebaceous gland. When a
hair has reached its full term of existence it falls, and is replaced by a
new hair formed around the old papilla, and whose growth has frequently
40 ANATOMY AND PHYSIOLOGY OF THE SKIN
started before the old hair has been entirely cast off, the latter often
being pushed out by the new growing hair.
The term bed hairs, so named by Unna, are those early or
embryonal hairs, unprovided with papilla, that push out from the
sides of shallow follicles from epithelial offshoots, and that fall out
and are supplanted by young papillary hairs, usually near the end
of intra-uterine life or shortly after birth.
The embryonal hairs are shed in utero, beginning with the seventh
or the eighth month, their place being taken by new hairs growing
in the same follicle; and if this hair-shedding, or normal hair change,
is not finished at birth, it completes itself in the first few months after
ward. The long black hairs on the scalp sometimes observed at birth
are in reality embryonal or
lanugo hairs, the shedding of
which has merely been post
poned until after birth.
There is some difference of
opinion as to the manner of
hair growth. C. Heitzmann
believes—and his view is shared
by Professor Duhring—that the
new growth takes place within
the province of the root-sheath
proper exclusively, being a pro
duct of the latter, the young
hairs, as shown by Kölliker
and Lang, forming around the
old papilla.
Hair-follicle.—The hair-
follicle or sac is the root-bed
of the hair, and consists of an
obliquely directed, pouch-like
depression in the skin, into the
central part of the base of
which projects the hair-papilla.
The follicle proper is usually considered to include, in its strictest limi
tation, all that part of the sac below the point of entrance of the seba
ceous duct, which is the narrowest part, or neck of the follicle; the outlet
above this, or the mouth of the follicle, is funnel shaped, and the part
below expands somewhat broadly down to the base. The sheaths of the
follicle, which is essentially a depression from the surface, practically
correspond to the epidermis and corium, the former representing the
inner coat and the latter the outer coat (C. Heitzmann). The accom
panying longitudinal and transverse sections of the follicle and inclosed
hair show the construction and the different layers of both of these
structures.
The dermic or external coat, which gives substantial and firm form
to the follicle, consists of bundles of connective-tissue fibers running
parallel to the follicle, with some elastic fibers, occasional muscular
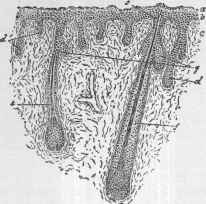
Fig. 18.—Section of skin of fetal kitten
exhibiting hairs in various stages of devel
opment: a, Superficial layers of epidermis;
b, rete mucosum, from which rudimentary
hair-follicles extend into connective tissue
(c) of the primitive corium; d,d,e,f,f, hairs
in different stages of development; g, seba
ceous glands growing from young hair-folli
cle (Piersol).
THE HAIR
41
fibers from the arrector pili, circularly disposed, and scanty fat-cells.
The outermost part (external layer) is richly supplied with blood-
vessels and some medullated nerve-fibers; the middle layer showing
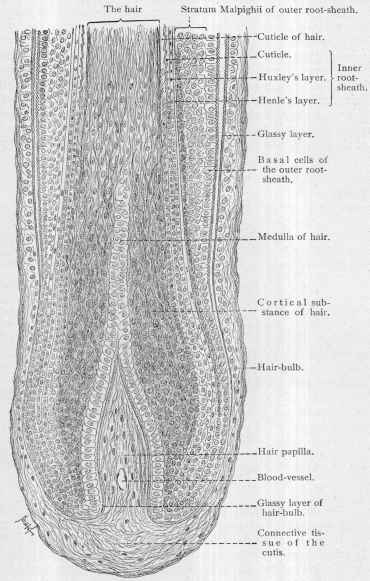
Fig. 19.—Longitudinal section of human hair and its follicle (X about 300) (Böhm
and Davidoff).
some capillaries, in the main transversely disposed, extends into the
papilla, and bears some resemblance to muscular tissue—so much so
that there is a difference of opinion regarding this point. The inner
42 ANATOMY AND PHYSIOLOGY OF THE SKIN
layer (internal layer) of the dermic coat, also known as the hyaline
or vitreous membrane or glassy layer, is of homogeneous structure, thin
at the upper portion of the follicle, becoming thicker as it approaches
the base, and thinning again as it nears the papilla.
The epidermic or inner coat, more generally known as the outer or
external root-sheath (Professor Duhring designates this the epidermis
of the hair-follicle, and Unna, the “prickle-cell layer of the hair-follicle”),
consists essentially of a turning inward of the rete, which, contiguous
to the inner or vitreous membrane of the dermic coat, dips downward,
lining the whole follicle, thinning at the base and into the neck of the
hair papilla as one or two rows of cells, and merging with those of other
layers. From this sheath the epithelial budding or pouch is produced,
which develops into the sebaceous gland. It is thickest at the middle
of the follicle, and is several times thicker than the root-sheath proper.
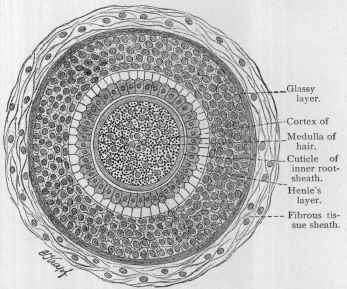
Fig. 20.—Cross-section of human hair with its follicle (X about 300) (Böhm and
Davidoff).
The root-sheath proper of the hair (Unna and Kölliker),
more generally known as the inner or internal root-sheath, has two
layers—an outer, or sheath of Henle, and an inner, or sheath of Huxley.
It arises from the cylindric cells covering the hair-papilla (Robinson).
As Macleod states, these layers are “only parts of a single layer, so
modified by differences in tension and pressure, and by the presence of
more or less keratohyalin in their cells, as to suggest that they have
had a different origin.” The former consists of pale and finely granular
polyhedral, somewhat elongated, non-nucleated epithelia, or with in
distinct nuclei. In the inner sheath the cells are coarsely granular and
nucleated. At the base of the follicle the sheath doubles on itself and
THE NAILS 43
surrounds the papilla; the cells are soft, broader, polygonal, and rounded,
contain granules of keratohyalin, and fuse with contiguous layers of the
hair, forming a broadened knob—the hair-bulb.
The root-sheath proper is covered with a closely adherent cuticular
membrane, with overlapping, shingle-like cells directed downward
(Ebner, cited by Duhring), the reverse of those of the hair cuticle, so
that the scales of these two contiguous layers interlock. As has been
stated previously, the hair is believed to be a solid elongation of this
root-sheath.
The Hair-papilla.—This is a club-shaped or spheric formation,
arising from the corium as a narrow neck-like projection or pedicle, and
expanding upward into the hair-bulb, by which it is surrounded. It is
about twice as long as it is broad, its breadth, according to Robinson,
being in direct proportion to the length of the hair. It is composed of a
delicate fibrous or myxomatous connective tissue, devoid of fibrillæ
and elastic fibers, freely supplied with colorless or pigmented connective-
tissue corpuscles, and containing a number of blood-vessels, with a
loop in its apex similar to that of the papilla of the corium. Knowledge
as to the nerve-supply of the hair-papilla is somewhat indefinite. Robin
son states that non-medullated nerve-fibers are to be found within its
structure; and according to Merkel, Ranvier, and Bonnet, nerves and
nerve-endings are observed in abundance close by in connection with the
follicle and its membranes.
THE NAILS
The nails are horny, elastic, transparent, shield-shaped, plate-like
formations, derived from the epidermis, embedded in the corium on
the dorsal aspect of the distal phalanges of the fingers and toes. They
are moderately curved downward from side to side, and less decidedly
from the root, or posterior part, to the anterior or free edge.
In substance a nail proper corresponds to the horny layer of the
epidermis, and differs from it only in being harder and firmer, with a
soft layer beneath, corresponding to the rete, constituting in reality a
part of the nail-bed. According to Bowen, it is a modification of the
stratum lucidum. It is made up of separate strata, composed of poly
gonal cells, or little plates, of which the lower ones exhibit indistinct
nuclei, the outermost resembling epidermal scales. Sometimes, in the
intercellular spaces, and also in the interior of the plates, small or large
air-vesicles occur, and produce by reflected light the so-called “white-
spots,” “gift spots,” etc
Various names are used to designate different portions of its sub
stance, and the couch or surface upon which it grows and rests.
The nail (unguis) is divided into two parts—the uncovered part, or
nail body, and the embedded portion, or nail-root. The former is usually
spoken of as the nail proper.
The top surface of the nail is smooth, horny, and glossy; the under
surface shows a number of longitudinal ridges, which, with the postero-
anterior papillary ridges of the underlying corium, form an interlocking,
44 ANATOMY AND PHYSIOLOGY OF THE SKIN
giving the nail a much firmer seat than if the under surface were smooth
and even. The nail is embedded posteriorly, and to some extent laterally,
into a depression between the matrix and overlapping skin, known as the
nail-groove, which also extends on upward along the free side; the over
lapping portion of skin is known as the nail-fold, or nail-wall, and the
thin, film-like layer of cuticle extending forward from the fold over the
body of the nail posteriorly for a short distance is the eponychium,
or nail-skin, whereas the epidermis bordering the whole nail is called the
perionychium, and that underlying the body of the nail upon which it
rests, the hyponychium.
The term nail-bed is usually employed to designate that part upon
which the uncovered portion of the nail rests, although in reality it
signifies the whole nail couch; that part, however, beneath the nail-
root, or embedded portion of the nail, is known as the matrix. These
two parts of the nail-couch are separated by the lunula, a more or less
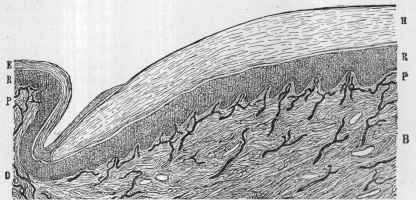
Fig. 21.—Nail (longitudinal section) (X 100): H, Nail-plate corresponding to
horny layers; R, R, rete mucosum; P, P. papillary layer; B, bed of nail; E, epidermis;
D, derma with injected blood-vessels; N. S, nail-skin; N. F, nail-fold; N. G, nail-groove
(L. Heitzmann).
convex line or half-moon-shaped area at the base of the uncovered por
tion, and that is most distinct on the thumb, although usually well
defined on the other fingers; it is often ill defined or absent on the toes,
although in many instances it becomes visible after the nail-fold has
been pushed back. There is some difference of opinion concerning its
formation. According to Hebra, it corresponds to a part of the matrix
or nail-couch devoid of papillae. Ranvier, Toldt, Duhring, Bowen, and
others ascribe it to opacity or decreased transparency of the nail-tissue
at this place. The latter seems to be the correct view; the opaque ele
ments are, according to Henle, Duhring, and others, transitional cells
thickly covered with points that by reflected light appear whiter than the
granular cells. Macleod thinks it is probably due to the presence of re
fractive keratohyalin granules in the transitional cells.
The nail-bed is formed of the rete, corium, and subcutaneous tissue,
and, in the region of the root of the nail, at the matrix, there is a gradual
THE NAILS 45
transformation from the epithelial cells of the rete into those of horny
character, resulting in the production of the hard-nail substance itself.
The rete layer of the epidermis constitutes the germ-layer of the nail or
the matrix, and this is the only part of the nail-couch that is concerned
in generating the nail. The subjacent papillary layer of the corium is
highly developed, especially the papillæ of the matrix. The papillæ
are shorter, broader, and more closely set in the matrix than anteriorly,
and in the former region project forward; they are arranged in parallel
rows longitudinally disposed, forming comb-like ridges that tend to
converge symmetrically in their posterior division.
The subcutaneous tissue underlying the corium contains no fat.
The ascending connective-tissue fibers arise from the periosteum of
the last phalanges, and extend in a brush-like manner toward the nail-
root, constituting the retinacula unguium of Kölliker. The nail-bed is
highly vascular, being well provided with blood-vessels, especially the
papillæ of the matrix. The nerve supply is not so abundant as that of
the surrounding skin.
The development of the nail begins in the third fetal month as a
fold in the epidermis. Before the end of the fourth month the entire

Fig. 22.—Section through dorsal portion of ungual phalanx of four-months’-old
fetus: c, Nail-bed; m, mucous layer; e, upper strata of mucous layers, showing cells
with eleidin-like granules; n, nail lamellae, ep, eponychium (Kölliker).
fingers and toes are covered with a continuous layer of “granular and
bladder cells,’’ representing, in the region of the nails, a persistent and
thickened portion of the epitrichial layer of the young embryos, and in
which region Unna has designated it the eponychium; beneath this the
nail makes its appearance, formed from peculiar cells in the upper part
of the rete containing deeply stained granules of keratohyalin (Bowen).
During the fifth month, Bowen further states, the epitrichial covering
of the nail, or the eponychium, is cast off from the body of the nail,
and the free surface exposed; whereas, at the edges the bladder and
granular cells are heaped up in great numbers in a ridge-like manner, and,
undergoing a process of keratosis, form a part of the normal stratum
corneum.
Nail-growth varies somewhat in different individuals and in different
nails; it is more rapid in the young and during the summer, and slower
in the nails of the toes than in those of the hands. Exposure of the
latter to light and air has probably a determining influence. According
46 ANATOMY AND PHYSIOLOGY OF THE SKIN
to Moleschott, the difference of rapidity in summer is much more
noticeable in the nails of the right hand. Berthold states that the growth
from the lunula to the free edge of the fingers requires an average of
about four months, and Dufour’s observations practically agree with this.
Quain gives a growth of 1/32 inch in a week. Moleschott found, from
observations on his own person, that the nails of the hands and feet to
gether produce about 9.2 milligrams of nail substance in a day, equiva
lent to about 3½ grams a year.
But first, if you want to come back to this web site again, just add it to your bookmarks or favorites now! Then you'll find it easy!
Also, please consider sharing our helpful website with your online friends.
BELOW ARE OUR OTHER HEALTH WEB SITES: |
Copyright © 2000-present Donald Urquhart. All Rights Reserved. All universal rights reserved. Designated trademarks and brands are the property of their respective owners. Use of this Web site constitutes acceptance of our legal disclaimer. | Contact Us | Privacy Policy | About Us |